Table of Contents:
- Pathogens – Unseen Troublemakers
- Infections – The Intruder Alert
- Spread of Disease – The Unwanted Sharing
- Immune Response – The Superhero Squad
- Vaccination – The Training Ground
- Antibiotics and Painkillers – The Support Team
- Antibiotic Resistance – The Super Villains
- Plant Diseases – Green Alert
- Discovery and Development of Drugs – The Grand Treasure Hunt
- Monoclonal Antibodies – The Custom-Made Protectors
- Test Yourself
- Additional Knowledge – GCSE Biology – Infection and Response
Pathogens – Unseen Troublemakers
Imagine a world where invisible creatures lurk, waiting for the chance to wreak havoc. It sounds like something from a superhero comic book, right? But guess what, it’s real! These troublemakers are called pathogens – the villains in our story of health.
Pathogens are like microscopic invaders. They’re not aliens from another planet, but they can feel just as foreign. They belong to four main groups: bacteria, viruses, fungi, and protists.
Let’s meet each of them.
- Bacteria: Think of these as the classic bandits. They’re single-celled organisms, pretty simple in construction. But don’t let their simplicity fool you! They reproduce very quickly and can form entire armies in your body within hours. For example, the bacteria Streptococcus pyogenes are the mischief-makers behind the annoying sore throat you get in tonsillitis.
- Viruses: These guys are the real stealthy ninjas. They’re even smaller than bacteria and not technically alive because they can’t do much on their own. But give them a host cell to take over, and boom! They’ll turn it into a virus-making factory. The infamous SARS-CoV-2, which causes COVID-19, is a prime example.
- Fungi: Fungi might remind you of mushrooms, the stuff on your pizza. But some fungi are more sinister. They’re more like squatters, settling on your skin or in your lungs, taking what they need, and causing discomfort or worse. Athlete’s foot is a common fungal infection that makes your feet itchy and uncomfortable. Not cool, fungi, not cool.
- Protists: Lastly, these are tiny organisms that often live in water. Most are harmless, but a few like to cause diseases. One such infamous protist is Plasmodium. A tiny mosquito bite can inject this protist into your blood, where it causes the severe and sometimes deadly disease known as malaria.
Pathogens enter our bodies, multiply, and interfere with our normal functions, causing what we call ‘disease.’ They might sound terrifying, but remember, our bodies are equipped with sophisticated defense systems to tackle these baddies. The more we learn about these microscopic invaders, the better we get at preventing their attacks and treating their mischief.
Infections – The Intruder Alert
Imagine your body as a high-tech, well-guarded fortress. You’ve got walls (skin), security personnel (immune cells), and a top-notch surveillance system (your immune response). Everything runs like clockwork until one day, the alarm bells start ringing. Intruders have been detected. Those intruders are pathogens, and they’ve just initiated an infection!
So, what exactly is an infection?
In the simplest terms, an infection is like a surprise party your body didn’t ask for. It happens when pathogens—those microbes we talked about earlier—manage to bypass your body’s defences, enter your body, and start to multiply. The party gets out of control, and suddenly, you’ve got more uninvited guests (pathogens) than your body can handle.
These pathogens can get in through various doorways: a cut on your skin, through the food or water you ingest, the air you breathe, or via an animal or insect bite. And once inside, they set up shop in your cells and tissues, and start to interfere with your body’s normal functions.
Let’s use the example of the flu, caused by the influenza virus. This virus is a master of disguise. It enters your body usually through your respiratory system when you inhale tiny droplets in the air that an infected person has coughed or sneezed out. Once inside, the virus invades your cells and turns them into tiny flu factories, churning out more and more viruses.
That’s when your body’s security team, the immune system, jumps into action. It tries to control the unruly crowd and clean up the mess. It’s your immune system’s response that often leads to the symptoms we associate with being sick, like fever, coughing, and feeling tired. These are signs that your body is fighting back, trying to evict the unwanted guests.
So, an infection is like an unwanted party happening in your body, causing chaos and disrupting the usual peace. But remember, you’ve got an entire team, your immune system, ready to control the situation and restore order. With their help, and sometimes with a boost from medicines or other treatments, you can kick out those gate crashers and get back to normal!
Spread of Disease – The Unwanted Sharing

Remember the old saying, “Sharing is caring”? Well, when it comes to diseases, sharing is definitely not caring. Diseases can spread from person to person in some unexpected and sneaky ways. This sharing of disease is called “transmission,” and it’s kind of like a hot potato game nobody wants to play.
In infection and response biology, learning how diseases spread is essential. Pathogens move in various ways:
Direct Contact
This is the equivalent of a high-five or a handshake between you and a pathogen, usually facilitated by an infected person. Catching a cold after hugging a sick friend or getting chickenpox from your sibling who’s broken out in those pesky spots are examples of direct contact transmission.
Airborne
Here, diseases fly first-class. Pathogens hitch a ride on tiny droplets that come out when an infected person coughs or sneezes. If you breathe in these droplets, you might catch the disease. The flu and COVID-19 spread this way.
Water and Food
Some pathogens prefer to go with the flow, contaminating the water you drink or the food you eat. If you’ve ever had food poisoning from that dodgy takeaway or a stomach bug from drinking unclean water, you’ve experienced this type of transmission.
Vectors
Some pathogens use living things like insects to move from one host to another. Think of it as a taxi service, with mosquitoes often playing the role of the cab. Malaria, dengue fever, and Lyme disease all spread this way.
Fomites
This is a fancy word for everyday objects that can carry pathogens. If an infected person sneezes on their hand and then touches a doorknob, that doorknob can become a fomite. When you touch the same doorknob and then touch your face, you can get infected.
Immune Response – The Superhero Squad
Ever wonder why, after feeling sick for a few days, you start to get better? That’s all, thanks to your personal superhero squad – the immune system! The immune response is at the heart of infection and response biology.
Imagine your body as a bustling city. All is well until one day, invaders (pathogens) sneak in, looking to cause trouble. Just like any great city, you’ve got a dedicated team ready to defend you. In this case, it’s not the police or firefighters; it’s your immune system.
First Responders – Innate Immunity
Just like firefighters are the first on the scene during a fire, your innate immune response is the first line of defence against invaders. This includes physical barriers like your skin, chemicals in your blood, and immune cells that attack all foreign substances. They don’t discriminate; if it’s foreign, it’s a foe.
Special Forces – Adaptive Immunity
When the threat is too big for the first responders alone, your immune system calls in the special forces. This includes white blood cells called T-cells and B-cells. They’re like elite soldiers, trained to recognize and remember specific pathogens. Once activated, T-cells destroy infected cells, and B-cells produce antibodies that neutralize the pathogens.
The Clean-Up Crew
Once the pathogens have been defeated, the immune system doesn’t just clock out and head home. There’s a clean-up phase, where dead cells and other debris from the battle are cleared away. Some immune cells ‘remember’ the invader, helping your body to respond more quickly if the same pathogen tries to invade again.
Think of the immune response like a well-coordinated defense operation, with different teams working together to protect the city (your body) from harm. They’re like superheroes, tirelessly working behind the scenes to keep you safe. This defence requires energy, which your body produces through cellular respiration, an essential process that powers all your body’s functions, including immune responses.
Next time you recover from a cold or a cut heals, take a moment to appreciate your internal superhero squad – the immune system. With them on your side, you’re more than ready to face any microscopic invaders!
Vaccination – The Training Ground
Ever wish you could see the future? When it comes to fighting diseases, your body kind of can, thanks to the miracle of vaccines!
A vaccine is like a training simulator for your immune system, preparing it for a fight before the real enemy shows up. Here’s how it works:
Training Day
A vaccine, which contains a weakened, dead, or partial version of a pathogen, is introduced into your body. Don’t worry, this mock enemy can’t make you sick, but it’s enough to make your immune system sit up and take notice.
Boot Camp
Your immune system swings into action, learning how to fight this new “intruder”. Special forces – your T-cells and B-cells – are recruited and trained to recognise this specific enemy. This immune response requires significant energy, produced through cellular respiration and other bioenergetic processes, to power the production and activation of these specialised cells.
Memory Cells
Some of these cells turn into memory cells. They’re like the old veterans sitting in the corner of the bar, telling stories about past battles. They remember the enemy, how it fights, and most importantly, how to defeat it.
Ready for Action
Now that your immune system has been trained, it’s ready for the real deal. If the actual pathogen tries to invade your body in the future, your immune system recognizes it, remembers how to fight it, and launches a faster and more effective attack. In many cases, this can prevent you from getting sick, or at least significantly reduce the severity of the disease.
Imagine being able to practice a video game level before playing it for real, or seeing the answers before a test. That’s what vaccines do for your immune system. They provide a safe and effective way to prepare for, and protect against, various diseases.
So, vaccines are like the ultimate prep course for your immune system, turning it into a well-prepared defense force ready to protect your body from specific diseases. With vaccination, you’re not just hoping for the best; you’re actively ready for the fight!
Antibiotics and Painkillers – The Support Team
Think of your body as a battlefield. When you’re sick, your immune system, the superhero squad, fights off the invading pathogens. But sometimes, even superheroes need a little help. Enter: the support team, which includes antibiotics and painkillers. These medicines aren’t the heroes of the story, but they play crucial roles in your body’s fight against disease.
Antibiotics – The Special Reinforcements
Antibiotics are like elite reinforcements called in to fight alongside your immune system, but they only join battles against bacteria. Imagine antibiotics as tiny soldiers, armed with specific weapons that can either kill bacteria or stop them from multiplying. They target processes that are unique to bacteria, which helps avoid damage to your body’s cells. For example, penicillin, one of the earliest antibiotics, blocks a substance bacteria need to build their cell walls, causing the bacterial cells to burst and die. But remember, antibiotics can’t distinguish between friendly and enemy bacteria, so they can sometimes disrupt the helpful bacteria in your body too.
Painkillers – The Medics
Now let’s talk about painkillers. They don’t fight the invaders, but they help manage the symptoms of the battle. Think of them as medics who take care of injured soldiers on the field, providing relief from symptoms like pain, fever, or inflammation. Painkillers like paracetamol or ibuprofen don’t cure the disease or kill pathogens; instead, they make you feel better while your immune system does the heavy lifting.
It’s important to remember that antibiotics should only be used when necessary and always under a doctor’s guidance, to avoid antibiotic resistance – a situation where bacteria evolve to withstand the weapons of the antibiotics. And while painkillers can help manage symptoms, they aren’t a solution to the underlying problem.
So, antibiotics and painkillers are like a support team, helping your immune system fight diseases more effectively and making the battle less uncomfortable for you. They’re not the main heroes, but they’re invaluable members of your healthcare squad!
Antibiotic Resistance – The Super Villains
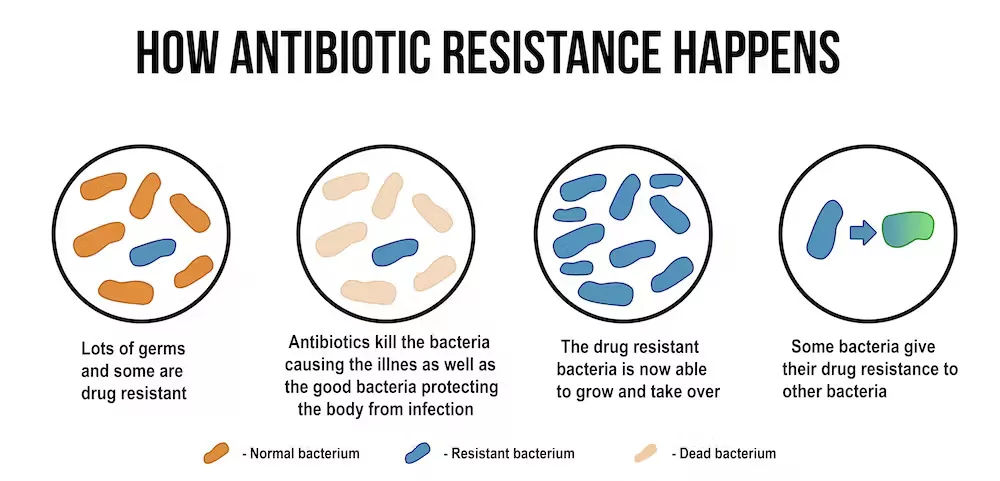
You know how in some movies, the villain comes back stronger after every defeat, seemingly invincible? This isn’t just a cinematic trope; it’s a real-world problem when it comes to antibiotics. Meet the super villains of our story: antibiotic-resistant bacteria.
Antibiotic resistance happens when bacteria evolve to outsmart the weapons we use against them – the antibiotics. Like any good villain, they adapt and learn, developing new ways to survive the attacks of antibiotics.
Here’s how it works:
- Survival of the Fittest: When you take an antibiotic, it kills off the bacteria that are sensitive to it. But some bacteria, by chance, might have genetic mutations that allow them to withstand the antibiotic. These ‘resistant’ bacteria survive.
- Rise of the Resistance: Now, with less competition around, these resistant bacteria multiply and spread. Suddenly, we’ve got a bunch of antibiotic-resistant bacteria on our hands, and our once-effective antibiotics can’t touch them.
- Sharing is Not Caring: What’s even worse is that bacteria can share these resistance traits with each other through something called horizontal gene transfer. It’s like one villain sharing their secret weapon with all the other villains.
So, how can we fight these super villains? Here are a few strategies:
- Responsible Use: Only use antibiotics when necessary and prescribed by a doctor. Always complete the full course, even if you’re feeling better, to ensure all bacteria are killed and none get a chance to develop resistance.
- Research and Development: Scientists are constantly researching to understand antibiotic resistance and develop new drugs to combat these superbugs.
- Prevention is Better than Cure: Vaccines can prevent bacterial infections from occurring in the first place, reducing the need for antibiotics. Good hygiene practices can also prevent the spread of resistant bacteria.
Antibiotic resistance is a major challenge, but by understanding it and tackling it responsibly, we can help slow down its spread. Just like in the movies, the battle against super villains isn’t easy, but with knowledge, strategy, and teamwork, we can fight back!
Plant Diseases – Green Alert
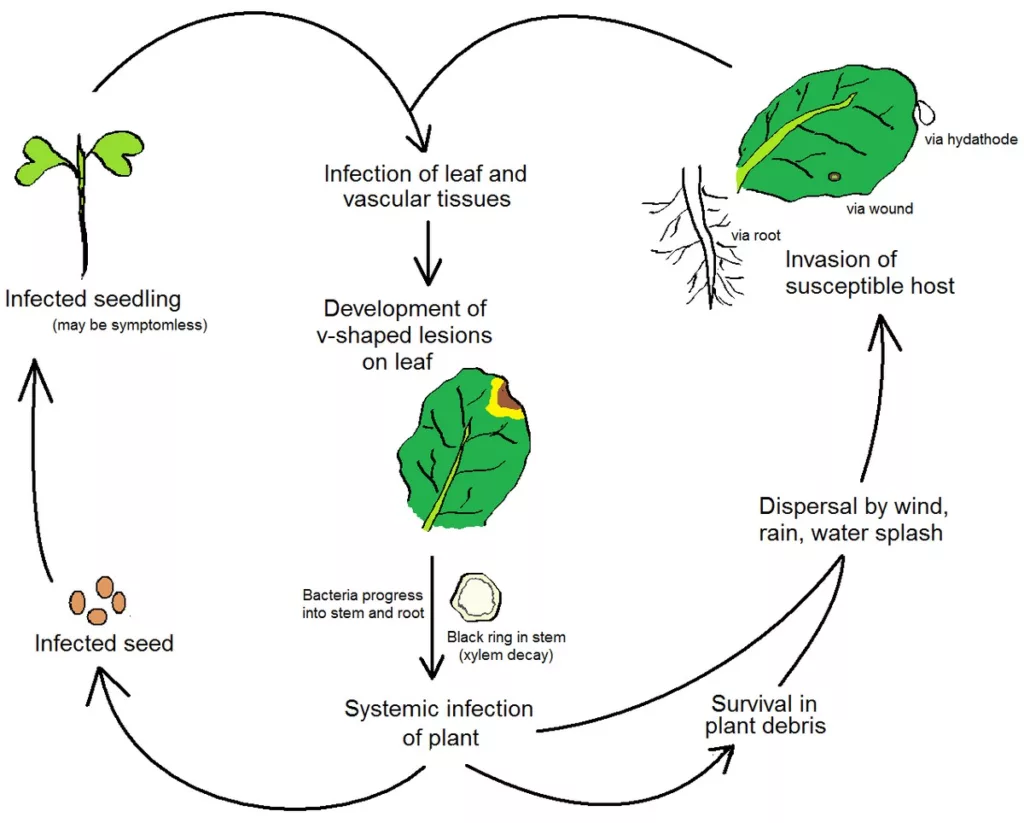
Just like us humans, plants can get sick too! They face threats from a variety of pathogens and can also suffer from nutrient deficiencies and physical damage. Think of this as a ‘green alert’, where our leafy friends need their own set of defenses and treatments to stay healthy.
So, what kind of illnesses do plants get?
- Infections: Plants can be invaded by a range of pathogens, including viruses, bacteria, and fungi. For example, the potato blight, a fungal disease, led to the Great Irish Famine in the 19th century. Another notorious plant disease is the Citrus Greening disease, caused by bacteria, which severely damages citrus crops worldwide.
- Pests: Plants are often attacked by pests like insects, which can damage their tissues, suck their sap, or act as vectors for disease. An infamous pest is the aphid, a small bug that sucks sap from plants and can transmit viruses between them.
- Nutrient Deficiencies: Just like us, plants need a balanced diet. They require various nutrients, including nitrogen, potassium, and phosphorus, which they usually get from the soil. If these are lacking, plants can exhibit a range of symptoms, like yellowing leaves (nitrogen deficiency) or poor flower and fruit growth (phosphorus deficiency).
So, how do plants deal with these problems?
- Built-In Defenses: Plants have several innate mechanisms to resist diseases, like tough cell walls, the ability to seal off and ‘quarantine’ infected areas, and even the production of certain chemicals that deter pests or kill pathogens.
- Human Intervention: Humans often help protect plants, especially in agriculture, by using methods like crop rotation, selective breeding for disease resistance, using pesticides to control pests, or adding nutrients to the soil.
In a nutshell, plant diseases are a significant issue, not just for the plants, but also for the ecosystems they belong to and the humans who depend on them for food, oxygen, and more. By understanding and managing plant diseases, we can help our green friends stay healthy and continue to support life on Earth!
Discovery and Development of Drugs – The Grand Treasure Hunt
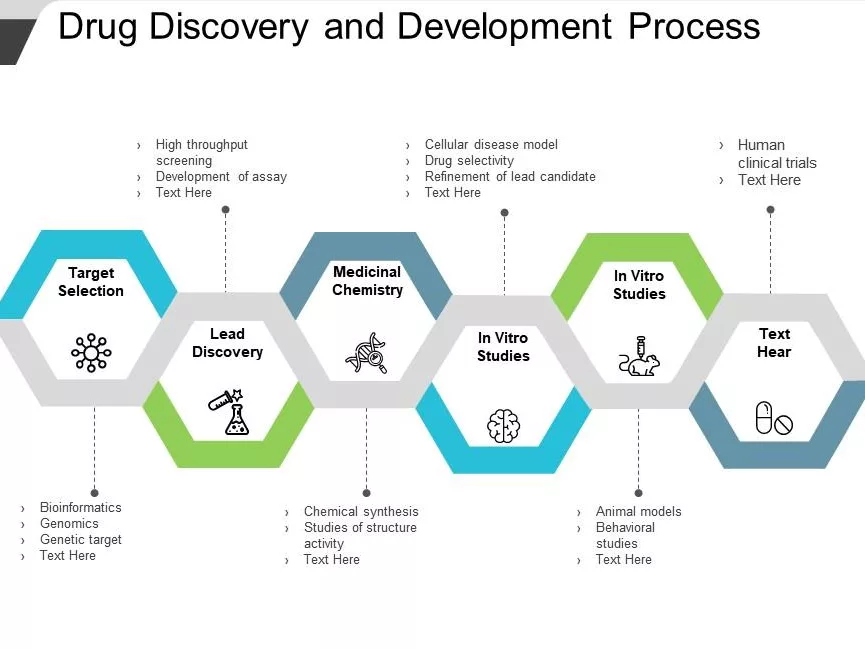
The journey to discover and develop new drugs is much like a grand treasure hunt. It involves explorers (scientists) searching through vast unknowns to find precious treasures (potential drugs), testing and refining these, and finally, ensuring they are safe and effective for use.
Here’s an overview of the process:
The Hunt Begins – Drug Discovery
The first step is identifying a target for a disease and then searching for potential drugs that can interact with this target. Scientists might screen thousands or even millions of chemical compounds, including naturally occurring substances and designed molecules, to find ‘hits’ that show promising activity. This is like searching a treasure map, looking for spots that might hide a valuable prize.
Refining the Treasure – Drug Design and Optimisation
Once potential hits are identified, they are optimized to improve their activity, selectivity, and safety. Chemists make small changes to the molecule’s structure to see how this affects its behavior. It’s like refining raw gold into a beautiful piece of jewelry.
Testing the Treasure – Preclinical Studies
The promising candidates then undergo extensive laboratory and animal testing to assess their safety, effectiveness, dosage, and potential side effects. This is the equivalent of appraising the jewelry to confirm its value and ensure it’s safe to wear.
The Final Hurdles – Clinical Trials
If a drug passes preclinical studies, it moves on to clinical trials in humans. These trials occur in phases, starting with a small group of volunteers and gradually involving more people. This helps to further determine the drug’s safety, effectiveness, and optimal dosage in humans. It’s like letting a few people try on the jewelry and then progressively more people, making sure it looks good and doesn’t cause any problems.
Approval and Monitoring
If the drug proves to be safe and effective in clinical trials, it can be approved for use in the general population. Even after approval, drugs are continually monitored for safety. It’s like the jewelry being made available for sale, but customers are asked to report any issues they encounter.
Remember, the process of drug discovery and development is long, complex, and requires a lot of resources, but it’s all worth it when a new drug is able to improve health and save lives. It’s a treasure hunt with the most rewarding prize – better health and wellbeing!
Monoclonal Antibodies – The Custom-Made Protectors
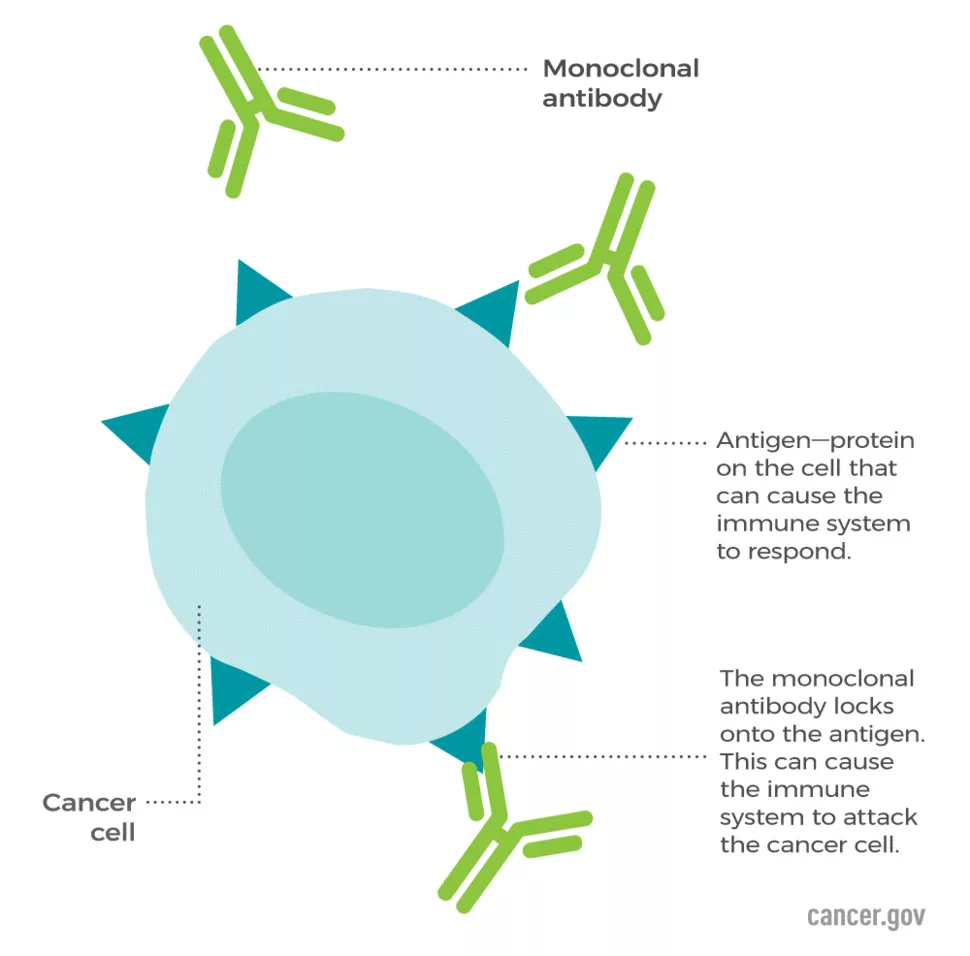
Picture a squad of expertly trained bodyguards, each one identical and specially equipped to recognize and neutralize a specific intruder. That’s essentially what monoclonal antibodies are in the realm of biology.
Here’s a simple explanation:
The Custom Design
Monoclonal antibodies are lab-made molecules designed to mimic the body’s natural antibodies, with one key difference: while natural antibodies can recognize many different foreign substances, each monoclonal antibody is tailor-made to recognize and bind to a specific target. This could be a particular molecule on a cancer cell, a specific protein on a virus, or even a molecule produced by the body itself in certain diseases.
The Production
To produce these identical antibodies, scientists first inject a mouse with the target molecule, prompting the mouse’s immune system to produce a range of antibodies. The cells producing the desired antibody are then fused with cancer cells to create ‘hybridoma’ cells, which can reproduce indefinitely in the lab, churning out large quantities of the desired antibody. It’s like creating an assembly line that only makes one very specific product.
The Mission
Once in the body, monoclonal antibodies work in various ways depending on their target. For instance, they can mark cancer cells for destruction by the immune system, block signals that tell cancer cells to grow, or deliver toxic substances directly to cancer cells. In the case of diseases like rheumatoid arthritis, they can bind to and neutralize overactive immune cells or proteins, causing inflammation. And in the case of viral infections, they can latch onto the virus and prevent it from entering human cells.
Monoclonal antibodies have transformed the treatment of many diseases, including various types of cancer, autoimmune diseases, and even infectious diseases. It’s like we’ve been able to train an army of bodyguards to recognise and neutralise specific threats to our health, providing us with a powerful tool in our medical arsenal.
Test Yourself
What is a pathogen? Give two examples.
A pathogen is a bacterium, virus, or other microorganism that can cause disease. Examples include the influenza virus and E. coli bacteria.
Explain the difference between bacteria and viruses.
Bacteria are single-celled microorganisms that can survive independently, while viruses are smaller and require a host cell to reproduce.
How does the immune system protect the body from pathogens?
The immune system uses various defenses, such as physical barriers (skin), chemical barriers (stomach acid), and cellular defenses (white blood cells) to identify, target, and eliminate pathogens.
What are antibiotics used for, and why don't they work on viruses?
Antibiotics are used to kill bacteria or inhibit their growth. They don’t work on viruses because viruses have a different structure and reproduce inside host cells.
Explain what antibiotic resistance is and why it's a significant concern.
Antibiotic resistance occurs when bacteria evolve to withstand the effects of an antibiotic. It’s a significant concern because it can make bacterial infections harder to treat.
How do vaccines work to protect individuals from specific diseases?
Vaccines introduce a weakened or inactive form of a pathogen into the body, triggering the immune system to produce a response, including the creation of memory cells. This prepares the immune system to fight off a future infection more effectively.
Describe the process of creating monoclonal antibodies.
To create monoclonal antibodies, researchers inject a mouse with a specific antigen. They then fuse the antibody-producing cells from the mouse’s spleen with cancer cells, creating a hybrid cell line (hybridoma) that produces large quantities of the desired antibody.
How can plant diseases be detected and treated?
Symptoms like discolouration, spots, or abnormal growth help detect plant diseases. You can treat them by removing infected parts, using chemical treatments, or planting disease-resistant varieties.
Explain the difference between active and passive immunity.
Active immunity is when the body’s immune system produces its own response to a pathogen (natural infection or vaccination), creating memory cells for future defense. Passive immunity is short-term, and involves the transfer of antibodies from another individual or species.
Why is drug testing an important part of the drug discovery and development process?
Drug testing is crucial to ensure the safety and efficacy of a new drug. It helps identify potential side effects, determine effective dosages, and ensure the benefits outweigh any risks.
Additional Knowledge – GCSE Biology – Infection and Response
GCSE Biology offers students an exciting opportunity to explore the complexities of living organisms and the natural world. This course delves into fundamental biological concepts, from the microscopic workings of cells to the vast interactions within ecosystems.
Students will develop a deeper understanding of life processes, genetic inheritance, and the intricate balance of ecosystems, while also honing critical scientific skills through experiments and real-world applications. Whether aspiring to a career in the sciences or simply wishing to understand the world better, GCSE Biology provides a solid foundation for future learning and discovery.
What is a pathogen?
A pathogen is a microorganism – such as a bacterium, virus, fungus, or protozoan – that causes disease in its host. They can invade the body and interfere with normal body functions, leading to an immune response and illness.
What’s the difference between bacteria and viruses?
Bacteria are single-celled organisms that can live in diverse environments, including within the human body. Some bacteria are beneficial, but others can cause diseases. Viruses, on the other hand, are much smaller and cannot survive without a host. They invade cells and use the cellular machinery to reproduce, often damaging or killing the host cells in the process.
What does the immune system do?
The immune system is the body’s defense mechanism against infections. It’s made up of a network of cells, tissues, and organs that work together to identify and destroy foreign invaders like bacteria and viruses, as well as the body’s own cells when they become damaged or diseased.
What are antibiotics and what do they do?
Antibiotics are medicines used to prevent and treat bacterial infections. They work by killing bacteria or preventing them from reproducing and spreading, but they’re not effective against viral infections.
What is antibiotic resistance and why is it a problem?
Antibiotic resistance occurs when bacteria evolve in a way that makes them immune to the effects of antibiotics. This can make bacterial infections much harder to treat, leading to higher medical costs, longer hospital stays, and increased mortality.
How do vaccinations work?
Vaccinations work by stimulating the immune system with an inactivated or weakened pathogen, or parts of the pathogen. This “teaches” the immune system to recognize the pathogen and respond quickly and effectively if the person is exposed to it in the future.
What causes plant diseases?
Plant diseases can be caused by various factors, including bacteria, viruses, fungi, and environmental conditions. Symptoms might include discolored leaves, wilting, stunted growth, and reduced yield or quality.
How are plant diseases treated or prevented?
Farmers can manage plant diseases by using disease-resistant plant varieties. They employ good agricultural practices, such as crop rotation and proper spacing, and apply chemical treatments or biological control methods.
What is a disease vector?
A disease vector is an organism that does not cause disease itself but spreads the infection by conveying pathogens from one host to another. Examples include mosquitoes, which can transmit diseases like malaria and dengue fever, and ticks, which can transmit Lyme disease.
What are non-specific defenses in the immune system?
Non-specific defenses are the body’s first line of defense against pathogens. They are called non-specific because they work against a wide range of pathogens. Examples include physical barriers like skin and mucous membranes, chemical barriers like stomach acid and enzymes in tears and saliva, and cells that respond quickly to any infection, such as macrophages and neutrophils.
What is an antigen?
An antigen is any substance that provokes an immune response when introduced into the body. Antigens are typically foreign substances, such as proteins on the surface of bacteria, viruses, and fungi.
What is the role of white blood cells in the immune response?
White blood cells, or leukocytes, play a key role in the immune response. Some, like phagocytes, ‘eat’ invading pathogens. Others, like lymphocytes, produce antibodies that target specific pathogens or release chemicals to regulate the immune response.
How are monoclonal antibodies produced?
Monoclonal antibodies are produced by creating hybridoma cells. This involves injecting a mouse with a target antigen, collecting the antibody-producing cells from the mouse’s spleen, and fusing these with myeloma (cancer) cells. The hybridoma cells can reproduce indefinitely in the lab, each producing the same specific antibody.
What is a pandemic?
A pandemic is an outbreak of a disease that occurs over a wide geographic area and affects an exceptionally high proportion of the population. The most well-known example in recent times is the COVID-19 pandemic caused by the SARS-CoV-2 virus.
Why can’t antibiotics be used to treat viral infections?
Antibiotics work by targeting specific structures or processes in bacteria. Since viruses have a different structure and replicate using the host cell’s machinery, antibiotics are ineffective against them.
What is the role of the memory cells in the immune system?
Memory cells are a type of lymphocyte that remain in the body long after an infection has been cleared. They ‘remember’ the specific antigens associated with that infection, enabling the immune system to respond quickly and powerfully if the same pathogen invades again, often preventing the disease from developing a second time.
What is a communicable disease?
A communicable disease, also known as an infectious disease, is caused by pathogens such as bacteria, viruses, parasites, or fungi that can be spread, directly or indirectly, from one person to another. Examples include the flu, tuberculosis, and HIV/AIDS.
What is an epidemic?
An epidemic is a rapid increase in the number of cases of a particular disease above what is normally expected in a population in a specific area.
What is herd immunity?
Herd immunity is a form of indirect protection from infectious diseases that occurs when a large percentage of a population has become immune to an infection, either through vaccination or previous infections, thereby providing a measure of protection for individuals who are not immune.
What is the difference between active and passive immunity?
Active immunity is long-lasting and is acquired by the immune response to a pathogen or vaccine. Passive immunity is short-term immunity that results from the introduction of antibodies from another person or animal.
Why is hygiene important in preventing disease?
Hygiene practices, such as regular hand washing and cleaning surfaces, help to remove or kill pathogens, reducing the risk of infection.
What are some ways diseases can spread?
Diseases can spread in many ways, including through physical contact, airborne droplets, contaminated food or water, sexual contact, blood transfusions, or from mother to child during birth.
What are some common types of plant diseases?
Common plant diseases include powdery mildew, rusts, leaf spot, and blights. They may be caused by a variety of pathogens, including fungi, bacteria, and viruses.
What are the different types of vaccines and how do they work?
There are several types of vaccines, including live-attenuated vaccines, inactivated vaccines, subunit or conjugate vaccines, and mRNA vaccines. Despite the differences, they all work by exposing the immune system to an antigen that will not cause disease but will provoke an immune response that can fight off that type of infection in the future.
What is the difference between an epidemic and a pandemic?
An epidemic is a disease outbreak that affects many people in a community or region at the same time. A pandemic is a global disease outbreak that affects people on a much wider scale, often worldwide.
What is meant by drug discovery and development?
Drug discovery and development refer to the processes that pharmaceutical companies use to discover new medicines and develop them into safe and effective treatments. This involves stages such as target identification, drug discovery, preclinical testing, clinical trials, and regulatory approval.
What are the symptoms that a plant is diseased?
Symptoms of plant diseases can vary widely but often include unusual discoloration (like yellowing or browning leaves), wilting, stunted growth, spots or blisters on leaves or stems, moldy coatings, and rotting plant parts.
Why is drug testing important?
Drug testing is important to ensure that new drugs are safe and effective before they are approved for use. It helps identify any potential side effects, understand the dosage at which the drug is effective, and ensure that its benefits outweigh any risks.
What is the role of T-cells and B-cells in the immune response?
T-cells and B-cells are types of white blood cells that play crucial roles in the immune response. B-cells produce antibodies that can bind to antigens and neutralize pathogens. T-cells can kill infected cells directly, and also help to regulate the immune response.
How can diseases be prevented?
Manage plant diseases by using disease-resistant plant varieties, employing good agricultural practices (like crop rotation and proper spacing), and applying chemical treatments or biological control methods.
What is drug resistance and why is it a problem?
Drug resistance occurs when pathogens evolve in a way that makes them immune to the effects of drugs that were previously effective. This can make infections much harder to treat, and is a major concern with diseases such as HIV, malaria, and tuberculosis.
What is a zoonotic disease?
A zoonotic disease is a disease that can be transmitted from animals to humans. These can be caused by viruses, bacteria, parasites, and fungi. Examples include rabies, Lyme disease, and some forms of influenza.
What is the difference between endemic, epidemic, and pandemic diseases?
Endemic diseases are those that are constantly present in a particular region or population, such as malaria in some parts of Africa. An epidemic is a sudden increase in the number of cases of a disease beyond what is normally expected in that population or area. A pandemic is a disease outbreak that occurs over a huge geographic area and affects a large proportion of the population, like the COVID-19 pandemic.
What are the primary and secondary responses in the immune system?
The primary response occurs when a pathogen enters the body for the first time. The immune system can take several days to fully respond, and in the meantime, the person may become sick. The secondary response occurs when the same pathogen enters the body again. Due to the memory cells produced during the first infection, this response is faster and stronger, preventing the person from getting sick again.
What is the role of the lymphatic system in immune response?
The lymphatic system plays a key role in the immune response. It transports and stores lymphocytes (white blood cells), carries the lymph fluid that contains these cells throughout the body, and filters out harmful substances like bacteria and toxins.
What is meant by ‘culture’ in the context of microbiology?
In microbiology, a culture refers to the growth of microorganisms in a nutrient medium (a substance that promotes growth), such as agar. Scientists can use cultures to study the characteristics of microorganisms and to identify pathogens.
What factors can contribute to the spread of diseases?
Many factors can contribute to the spread of diseases, including poor hygiene, lack of access to clean water or healthcare, close contact with infected individuals or animals, travel, and environmental changes.
What is the difference between active and passive immunity?
Active immunity arises when the body’s immune system responds to antigens by producing antibodies and memory cells. This can occur through natural infection or vaccination. Passive immunity arises from the receipt of pre-made antibodies, such as through breastfeeding or an injection of antiserum, and is temporary because the recipient’s body is not actively producing the antibodies.
How can monoclonal antibodies be used in medicine?
In medicine, people can use monoclonal antibodies in various ways, including treating diseases like cancer. They can design these antibodies to bind specifically to cancer cells and kill them or block their growth. People can also use them in diagnostic tests, like pregnancy tests, where they bind to specific hormones and create a visible signal.
How can the overuse or misuse of antibiotics lead to antibiotic resistance?
The overuse or misuse of antibiotics can expose bacteria to sub-lethal doses of the drug, promoting the survival of resistant bacteria. These resistant bacteria multiply and spread, leading to antibiotic resistance. This is why it’s important to use antibiotics only when necessary and to always complete the prescribed course.