Structure of The Heart (A-level Biology)
The heart is the central organ of the circulatory system, responsible for pumping blood throughout the body. The body continuously moves oxygen, nutrients, and hormones to every cell while efficiently removing waste products like carbon dioxide.. As the driving force behind circulation, the heart maintains the vital balance necessary for life, supporting everything from basic cellular functions to complex organ systems.
For A-level Biology students, understanding the heart’s anatomy and physiology is fundamental. This knowledge lays the groundwork for exploring broader topics such as the circulatory system, homeostasis, and cardiovascular health. By delving into the intricacies of heart structure and function, students not only develop a deeper appreciation of biological processes but also enhance their ability to apply this understanding to real-world contexts, such as interpreting medical conditions or advancements in heart-related research.
Anatomy of the Heart

External Features
To begin with, The heart is a muscular organ roughly the size of a closed fist, located in the thoracic cavity between the lungs, slightly tilted towards the left. It sits in a space called the mediastinum, resting on the diaphragm. Its orientation allows efficient blood flow to and from the lungs and the rest of the body, with the apex (pointed end) directed downward, forward, and to the left, while the broader base lies upward, near the second rib.
To protect and support this vital organ, the heart is encased in a double-layered sac known as the pericardium. The pericardium consists of two layers:
- Fibrous Pericardium: A tough, outer layer that anchors the heart in place and prevents overexpansion during vigorous activity or changes in blood volume.
- Serous Pericardium: A thinner, inner layer composed of two parts:
- Parietal Layer: Lines the inside of the fibrous pericardium.
- Visceral Layer (Epicardium): Directly covers the surface of the heart.
Between these layers is the pericardial cavity, filled with a small amount of lubricating fluid. Moreover, this fluid minimises friction as the heart contracts and relaxes, ensuring smooth and efficient movement. These protective structures are critical for maintaining the heart’s function and safeguarding it from physical trauma or infection.
Internal Structures of the Heart
The heart’s internal anatomy is intricately designed to ensure the efficient circulation of blood. It is divided into four chambers, separated by partitions and regulated by valves to maintain unidirectional blood flow.
Four Chambers
- Right Atrium: Receives deoxygenated blood from the body via the superior and inferior vena cava. It serves as the starting point for blood entering the heart.
- Right Ventricle: Pumps deoxygenated blood to the lungs through the pulmonary arteries for oxygenation.
- Left Atrium: Receives oxygenated blood from the lungs via the pulmonary veins.
- Left Ventricle: Pumps oxygenated blood to the rest of the body through the aorta. This chamber has the thickest walls to generate the high pressure required for systemic circulation.
Septum
The heart is divided into two halves by muscular partitions:
- Interatrial Septum: Separates the right and left atria.
- Interventricular Septum: Divides the right and left ventricles. These septa prevent the mixing of oxygenated and deoxygenated blood, ensuring efficient circulation.
Heart Valves
Valves within the heart maintain unidirectional blood flow and prevent backflow:
- Tricuspid Valve: Located between the right atrium and right ventricle, allowing blood to flow into the ventricle during atrial contraction.
- Bicuspid (Mitral) Valve: Found between the left atrium and left ventricle, functioning similarly to the tricuspid valve but on the left side.
- Pulmonary Semilunar Valve: Situated at the entrance of the pulmonary artery, it effectively prevents backflow into the right ventricle, especially after blood has been ejected to the lungs.
- Aortic Semilunar Valve: Located at the base of the aorta, it effectively prevents blood from flowing back into the left ventricle after it has been pumped into the systemic circulation.
Major Blood Vessels
The heart connects to large blood vessels that facilitate blood flow to and from the body and lungs:
- Vena Cava: Comprising the superior and inferior vena cava, these veins bring deoxygenated blood from the body to the right atrium.
- Pulmonary Arteries: Transport deoxygenated blood from the right ventricle to the lungs for oxygenation.
- Pulmonary Veins: Carry oxygenated blood from the lungs to the left atrium.
- Aorta: The largest artery, it distributes oxygenated blood from the left ventricle to the rest of the body.
Together, these structures enable the heart to function as a highly efficient pump, maintaining the circulation required for sustaining life.
Blood Flow Through the Heart
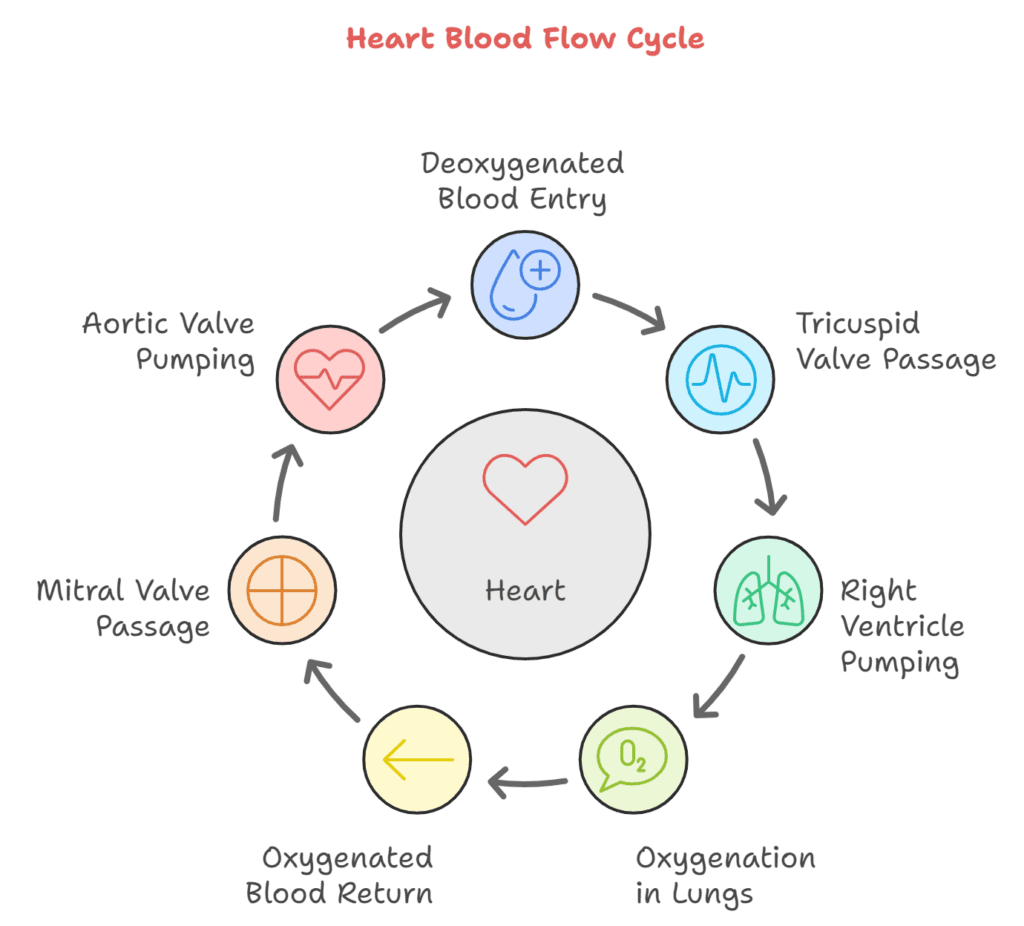
The heart ensures the continuous flow of blood, delivering oxygen and nutrients to the body while removing waste products. Its dual-pump structure supports two pathways: the pulmonary circuit for oxygenation and the systemic circuit for distribution.
Pathway of Deoxygenated Blood from the Body to the Lungs
- Deoxygenated blood from the body enters the right atrium via the superior vena cava (from the upper body) and inferior vena cava (from the lower body).
- During atrial contraction, blood flows through the tricuspid valve into the right ventricle.
- Upon ventricular contraction, the pulmonary semilunar valve opens, allowing blood to be ejected into the pulmonary arteries.
- The pulmonary arteries carry the blood to the lungs, where it becomes oxygenated during gas exchange.
Pathway of Oxygenated Blood from the Lungs to the Body
- Oxygenated blood from the lungs returns to the left atrium through the pulmonary veins.
- During atrial contraction, blood flows through the bicuspid (mitral) valve into the left ventricle.
- Upon ventricular contraction, the aortic semilunar valve opens, and blood is pumped into the aorta.
- The aorta distributes the oxygen-rich blood to the rest of the body via systemic arteries.
Role of Valves in Preventing Backflow
The heart’s valves play a crucial role in maintaining unidirectional blood flow:
- The tricuspid and bicuspid (mitral) valves prevent backflow into the atria when the ventricles contract.
- The pulmonary and aortic semilunar valves prevent blood from flowing back into the ventricles after it has been pumped into the pulmonary arteries or aorta.
By seamlessly coordinating with the cardiac cycle, these valves not only ensure efficient circulation but also effectively prevent the mixing of oxygenated and deoxygenated blood, thereby enabling the heart to function optimally as a pump.
The Cardiac Cycle

The cardiac cycle is a continuous series of events during a single heartbeat, ensuring the efficient circulation of blood. It comprises three main phases: atrial systole, ventricular systole, and diastole. These phases are driven by pressure changes within the heart’s chambers and coordinated by its electrical conduction system.
Phases of the Cardiac Cycle
- Atrial Systole:
- As the atria contract, they increase pressure, thereby pushing blood into the relaxed ventricles through the open tricuspid and bicuspid (mitral) valves.
- This phase ensures the ventricles are filled with blood before they contract.
- Ventricular Systole:
- As the ventricles contract, the pressure within them increases. Consequently, this causes the tricuspid and bicuspid valves to close, thereby preventing backflow into the atria.
- As the pressure rises, it subsequently forces the pulmonary and aortic semilunar valves to open, thereby ejecting blood into the pulmonary arteries and aorta, respectively.
- Diastole:
- Both the atria and ventricles relax, allowing blood to flow into the atria from the vena cava and pulmonary veins.
- As the ventricular pressure drops, the semilunar valves consequently close, effectively preventing any backflow from the pulmonary arteries and aorta.
- The tricuspid and bicuspid valves reopen as atrial pressure increases, restarting the cycle.
Pressure Changes and Their Effects on Blood Movement
- Blood flows from regions of higher pressure to lower pressure.
- During systole, the contraction of atria or ventricles increases pressure, propelling blood forward.
- During diastole, the relaxation of the chambers lowers pressure, allowing blood to flow into the heart from the veins.
- The opening and closing of valves are pressure-driven, ensuring unidirectional blood flow.
Heart Sounds and Their Physiological Origins
The heart produces two main sounds during each cycle, commonly described as “lub-dub”:
- First Heart Sound (S1): The “lub” sound occurs when the tricuspid and bicuspid valves close at the start of ventricular systole.
- Second Heart Sound (S2): The “dub” sound occurs when the pulmonary and aortic semilunar valves close at the start of diastole.
These sounds are produced by the sudden deceleration of blood flow and, consequently, the vibration of valve leaflets and surrounding structures, thereby providing key indicators of heart function. Irregularities in these sounds can signal potential cardiac issues, such as valve disorders.
The precise coordination of the cardiac cycle ensures the heart functions efficiently as a pump, maintaining the body’s circulatory needs.
Electrical Conduction System

The heart’s electrical conduction system, therefore, ensures that it beats rhythmically and efficiently, pumping blood throughout the body. Moreover, this system generates and transmits electrical impulses, effectively coordinating the contraction and relaxation of the heart’s chambers.
Sinoatrial (SA) Node: The Heart’s Natural Pacemaker
The SA node, located in the wall of the right atrium near the superior vena cava, is the heart’s primary pacemaker. Specifically, it generates regular electrical impulses, typically 60-100 times per minute in a healthy adult. Subsequently, these impulses:
- Initiate each heartbeat.
- Spread rapidly through the walls of both atria, causing them to contract (atrial systole) and push blood into the ventricles.
Atrioventricular (AV) Node
The electrical impulse from the SA node reaches the AV node, located at the junction between the atria and ventricles. The AV node acts as a gatekeeper:
- It briefly delays the impulse to ensure the ventricles have time to fill with blood after atrial contraction.
- It then passes the signal to the ventricles.
Bundle of His and Purkinje Fibres
From the AV node, the impulse travels along the Bundle of His, a specialised group of fibres located in the interventricular septum. Subsequently, the Bundle of His divides into:
- Right and Left Bundle Branches: These pathways transmit the signal down the interventricular septum.
- Purkinje Fibres: These fibres spread throughout the ventricular walls, delivering the impulse to the cardiac muscle cells.
This coordinated transmission ensures the ventricles contract simultaneously, pumping blood efficiently into the pulmonary arteries and aorta.
Coordination of Heartbeats and Maintenance of Rhythm
The entire electrical system ensures a precise sequence of events:
- The SA node sets the rhythm by initiating the impulse.
- The atria contract first, filling the ventricles with blood.
- The AV node delays the signal slightly, ensuring the ventricles are full.
- The signal then spreads through the Bundle of His and Purkinje fibres, causing the ventricles to contract simultaneously.
This system maintains a steady heart rhythm, adapting as needed during exercise, stress, or rest. Disruptions to this system, such as arrhythmias or heart block, can impair the heart’s ability to pump blood effectively, highlighting its vital role in cardiac function.
Coronary Circulation
The heart, much like any other organ, critically requires its own blood supply to function effectively. Consequently, this is ensured by the coronary circulation, which includes both coronary arteries and veins specifically dedicated to nourishing the heart muscle (myocardium) and efficiently removing waste products.
Coronary Arteries
The coronary arteries, therefore, originate from the base of the aorta, just above the aortic semilunar valve, and subsequently branch out to supply oxygen-rich blood to the myocardium. Specifically, the two main coronary arteries are:
- Left Coronary Artery (LCA):
- Divides into the left anterior descending (LAD) artery and the circumflex artery.
- Supplies blood to the left atrium, left ventricle, and a portion of the right ventricle.
- The LAD is often referred to as the “widow-maker” artery because blockages here can lead to severe heart attacks.
- Right Coronary Artery (RCA):
- Supplies blood to the right atrium, right ventricle, and portions of the left ventricle.
- Includes the posterior descending artery (PDA), which provides blood to the posterior part of the heart.
Coronary Veins
After oxygen is delivered to the heart muscle, deoxygenated blood is collected by coronary veins, which drain into the coronary sinus. The coronary sinus then empties the blood directly into the right atrium for reoxygenation. Key veins include:
- Great Cardiac Vein: Drains the areas supplied by the LCA.
- Middle Cardiac Vein: Drains the posterior heart regions.
- Small Cardiac Vein: Drains parts of the RCA territory.
Significance in Maintaining Cardiac Health
Coronary circulation is crucial for the heart’s health and performance:
- Oxygen and Nutrient Delivery: The heart requires a continuous supply of oxygen and nutrients to sustain its constant contractions.
- Waste Removal: Efficient removal of carbon dioxide and metabolic by-products ensures optimal cellular function.
- Cardiovascular Diseases: Any disruption in coronary circulation, such as blockages or narrowing of the coronary arteries (atherosclerosis), can lead to conditions like:
- Angina: Chest pain due to reduced blood flow.
- Myocardial Infarction (Heart Attack): Complete blockage causing damage to heart tissue.
- Heart Failure: Chronic inadequate blood supply weakening the heart.
Maintaining a healthy lifestyle – regular exercise, a balanced diet, and avoiding smoking—can significantly reduce the risk of coronary artery disease and promote efficient coronary circulation, ensuring the heart remains robust and functional.
Conclusion
Understanding the heart A level biology, cardiac cycle A level biology, and heart diagram A level biology is essential for mastering A-Level Biology. Whether revising diagrams, the cardiac cycle, or preparing for exams, if you’re seeking personalised guidance, Edumentors connects you with expert tutors who can simplify complex topics and boost your confidence. Whether you need help with diagrams, the cardiac cycle, or exam preparation, our tutors are here to support your academic success.
Blogs Which Can Help
How to Revise Biology? – Here is Top 10 Tips
AQA A-level and AS Biology Specification
A-level Biology Past Papers – OCR, AQA, Edexcel